Understanding Ovarian Cancer and Its Risks
Ovarian cancer, a malignancy that originates in the ovaries, represents a significant health concern for women worldwide. According to data, it is estimated that approximately 1 in 78 women will be diagnosed with ovarian cancer in their lifetime. This type of cancer can be particularly insidious; it often presents no obvious symptoms in its early stages, which can lead to delayed diagnosis and treatment. Common symptoms include abdominal bloating, pelvic pain, difficulty eating, and frequent urination. However, these manifestations can be easily overlooked or attributed to other health issues, underscoring the need for heightened awareness.
There are several types of ovarian cancer, including epithelial ovarian cancer, germ cell tumors, and stromal tumors, with epithelial ovarian cancer being the most prevalent. The risk of developing ovarian cancer varies based on various factors, including age, family history, genetic mutations, and lifestyle choices. Women with a family history of ovarian or breast cancer should consider early cancer detection strategies, as they may carry genetic mutations that significantly increase their risk.
Genetics play a crucial role in ovarian cancer risk, particularly mutations in the BRCA1 and BRCA2 genes. Women with these mutations have a substantially higher likelihood of developing ovarian cancer, as well as breast cancer. As a result, awareness about ovarian cancer and its risk factors is vital, especially for those with a family history of such conditions. Incorporating cancer prevention tips into one’s daily routine can be instrumental in reducing overall cancer risk. Maintaining a healthy lifestyle for cancer prevention, such as engaging in regular physical activity, adopting a balanced diet rich in fruits and vegetables, and minimizing alcohol consumption, can also play a role in mitigating risks.
The Role of BRCA Genes and Genetic Testing
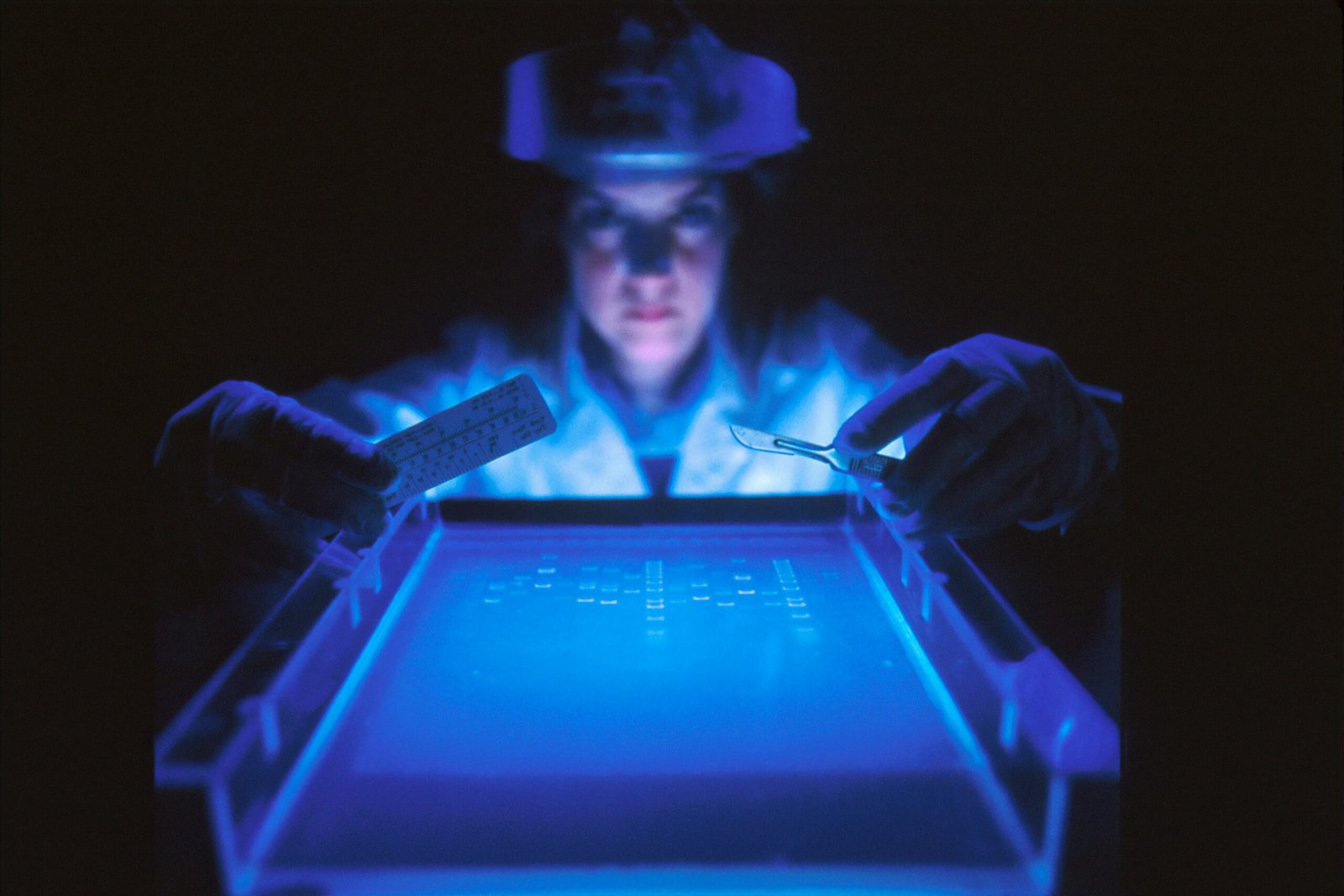
Understanding the role of BRCA1 and BRCA2 genes is crucial in the discussion of ovarian cancer and its prevention. These genes are involved in the repair of DNA breaks, and mutations in them can significantly impair the cell’s ability to manage genetic damage. Women who inherit harmful mutations in these genes face a considerably heightened risk of developing ovarian and breast cancer. Studies have shown that approximately 12% of women in the general population will develop ovarian cancer by the age of 80, but this rate soars to 44% for those with a BRCA1 mutation and 17% for BRCA2 mutation carriers.
Genetic testing plays an essential role in early cancer detection, as it helps identify high-risk individuals who may benefit from proactive measures. By undergoing genetic testing, women can know their status regarding these mutations, which allows for informed decision-making about their health. For instance, women identified as carriers may choose to engage in enhanced screening practices or consider preventive measures, such as prophylactic surgeries, significantly reducing their risk of developing cancer.
Case studies illustrate the profound impact of genetic testing. Take the example of Emily, a 34-year-old woman who learned she had a BRCA1 mutation through genetic testing. Armed with this knowledge, she opted for regular screening and ultimately decided to undergo a preventive oophorectomy, greatly reducing her risk of ovarian cancer. Emily’s story, along with many others, highlights the potential of genetic testing in cancer prevention. Women like her demonstrate that a proactive approach, supported by genetic insights, can lead to a healthy lifestyle for cancer prevention.
In conclusion, the identification of BRCA mutations through genetic testing serves not only as a tool for early cancer detection but also empowers women to make informed choices regarding their health and wellbeing.
Discussing Family Health History with Doctors
Understanding one’s family health history is a vital component of proactive healthcare, particularly concerning conditions such as ovarian cancer. Women should feel empowered to discuss their genetic background with healthcare providers as it can significantly influence early cancer detection. By initiating these conversations, patients can help their doctors assess their personal risk factors effectively.
When meeting with a healthcare professional, it is essential to prepare relevant information regarding family members who have been diagnosed with cancer. This includes not just immediate relatives like parents and siblings, but also extended family members such as grandparents, aunts, uncles, and cousins. Specific details to share include the types of cancer diagnosed, the ages at which family members received their diagnoses, and any other health conditions that may have occurred. This comprehensive overview can provide invaluable insight into hereditary patterns that may predispose someone to cancer, enabling timely and appropriate screening and preventive measures.
Women should feel comfortable inquiring about the implications of their family history. Questions might include, “Given my family history, are there particular screening tests I should prioritize?” or “What steps can I take to lower my risk of ovarian cancer?” Such inquiries not only allow for personalized medical advice but also facilitate discussions about lifestyle changes that can contribute to cancer prevention. These changes might encompass maintaining a healthy lifestyle for cancer prevention through dietary adjustments, regular exercise, and stress management strategies.
Utilizing family health history in conversations with healthcare providers not only emphasizes the importance of early cancer detection but also highlights the role of informed decision-making in cancer prevention strategies. Ultimately, understanding one’s genetic lineage can lead to crucial interventions that may save lives.
Healthy Lifestyle Choices for Cancer Prevention
Maintaining a healthy lifestyle can significantly contribute to cancer prevention, including the various forms of ovarian cancer. One of the foundational aspects of a healthy lifestyle is proper nutrition. A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can provide essential nutrients that help the body function optimally and may protect against certain cancers. Specifically, foods high in antioxidants, such as berries, nuts, and leafy greens, have been shown to combat oxidative stress, which can lead to cancer development.
Regular physical activity is another critical component of a healthy lifestyle for cancer prevention. Engaging in at least 150 minutes of moderate exercise, or 75 minutes of vigorous activity weekly, can help maintain a healthy weight and reduce overall cancer risk. Exercise not only supports weight management but also helps regulate hormones and boosts the immune system, both of which are vital in reducing the likelihood of cancerous changes in the body.
Avoiding known carcinogens is also essential for minimizing cancer risk. Lifestyle choices such as avoiding tobacco products, limiting alcohol consumption, and steering clear of environmental toxins can significantly lower the chances of developing cancer. It is vital to be mindful of exposure to substances that may increase cancer susceptibility and to adopt measures that limit such exposure.
In addition to maintaining a healthy diet and staying active, regular screenings and self-examinations play a crucial role in early cancer detection. Individuals, particularly those with a family history of cancer, should consult with healthcare professionals to establish a routine for screenings appropriate to their risk levels. These proactive health choices not only enhance overall well-being but can also significantly reduce the risk of cancer through early detection and intervention.
